Sepsis is a life-threatening medical condition that occurs when the body’s response to an infection spirals out of control. While sepsis can affect individuals of all ages, the elderly population is particularly vulnerable, as their weakened immune systems and underlying health conditions make them more susceptible to this potentially deadly condition. As a caregiver, it is essential to be aware of the unique symptoms of sepsis in the elderly and to act quickly to seek prompt medical attention.
Understanding Sepsis: Definition and Importance
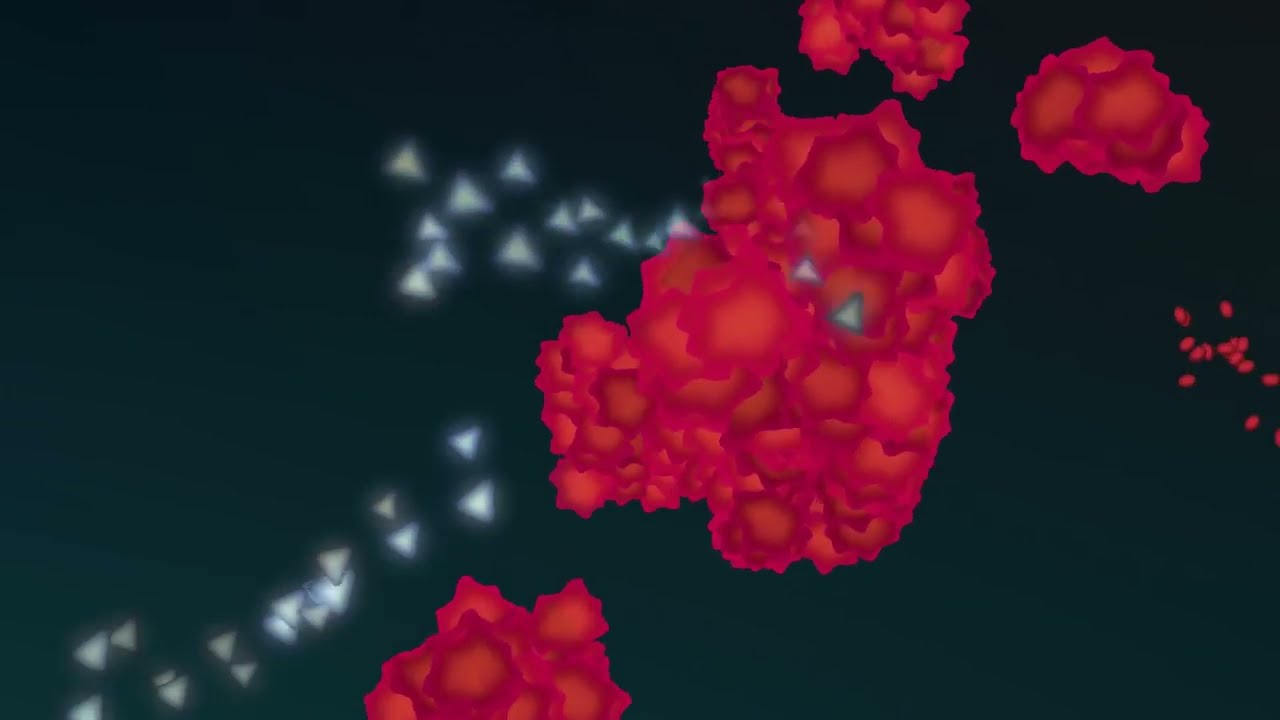
Sepsis is a complex and potentially fatal condition that arises when the body’s immune system overreacts to an infection, triggering a chain reaction of inflammatory responses that can lead to tissue damage, organ failure, and even death. It is a medical emergency that requires immediate treatment to prevent further complications and improve the patient’s chances of survival.
The Prevalence of Sepsis in the Elderly
Sepsis is a significant health concern for the elderly population, as they are at a higher risk of developing the condition due to a variety of factors, including:
- Weakened immune system: As we age, our immune system becomes less effective at fighting off infections, making the elderly more susceptible to developing sepsis.
- Underlying health conditions: Many older adults have chronic illnesses, such as diabetes, heart disease, or cancer, which can increase their vulnerability to infections and subsequent sepsis.
- Reduced mobility: Decreased physical activity and mobility can make the elderly more prone to developing infections, such as pneumonia or urinary tract infections, which can lead to sepsis.
- Medication use: The elderly often take multiple medications, some of which can weaken the immune system or mask the early signs of sepsis.
The Importance of Early Recognition and Treatment
Prompt recognition and treatment of sepsis are crucial, as the condition can progress rapidly and lead to life-threatening complications. Early intervention can significantly improve the patient’s chances of survival and reduce the risk of long-term complications, such as organ damage or disability.
Common Symptoms of Sepsis in the Elderly
Recognizing the symptoms of sepsis in the elderly can be challenging, as they may present differently or be more subtle compared to younger individuals. It is essential for caregivers to be aware of the following common signs and symptoms of sepsis in older adults:
Changes in Mental Status
Altered mental status is a common and often early sign of sepsis in the elderly. Older adults may experience confusion, disorientation, or even delirium, which can manifest as:
- Sudden changes in behavior or mood
- Difficulty concentrating or paying attention
- Confusion about time, place, or personal identity
- Agitation or restlessness
Fever or Hypothermia
While a fever is a common symptom of sepsis, the elderly may also present with hypothermia (low body temperature) due to their diminished ability to regulate body temperature. Caregivers should monitor the patient’s temperature and be aware of both high and low readings.
Respiratory Distress
Sepsis can lead to respiratory problems, such as rapid or shallow breathing, shortness of breath, or the need for increased oxygen support. Older adults may also exhibit signs of pneumonia or respiratory failure.
Cardiovascular Changes
Sepsis can cause cardiovascular instability, leading to changes in blood pressure, heart rate, and circulation. Caregivers should monitor the patient’s vital signs, including:
- Hypotension (low blood pressure)
- Tachycardia (rapid heart rate)
- Weak or rapid pulse
Altered Gastrointestinal Function
Sepsis can affect the gastrointestinal system, causing symptoms such as nausea, vomiting, diarrhea, or abdominal pain. Older adults may also experience decreased appetite or altered bowel habits.
Impaired Kidney Function
Sepsis can lead to impaired kidney function, which may be indicated by decreased urine output, darkened or bloody urine, or increased levels of waste products in the blood.
Skin Changes
Sepsis can cause changes in the skin, such as redness, warmth, or the development of a rash or mottled appearance. The elderly may also experience delayed capillary refill, which can be a sign of poor circulation.
Fatigue and Weakness
Older adults with sepsis may experience overwhelming fatigue, weakness, or decreased physical activity, making it difficult for them to perform their usual daily tasks.
By being aware of these common symptoms, caregivers can help identify sepsis in the elderly and seek prompt medical attention, which is essential for improving outcomes and reducing the risk of serious complications.
Risk Factors and Causes in Older Adults
Older adults face a higher risk of developing sepsis due to a variety of factors, including:
Weakened Immune System
As we age, our immune system becomes less effective at fighting off infections, making the elderly more susceptible to developing sepsis.
Underlying Health Conditions
Many older adults have chronic illnesses, such as diabetes, heart disease, or cancer, which can increase their vulnerability to infections and subsequent sepsis.
Reduced Mobility and Frailty
Decreased physical activity and mobility can make the elderly more prone to developing infections, such as pneumonia or urinary tract infections, which can lead to sepsis.
Malnutrition and Dehydration
Older adults may be at risk of malnutrition and dehydration, which can weaken their immune system and make them more susceptible to infections and sepsis.
Medication Use
The elderly often take multiple medications, some of which can weaken the immune system or mask the early signs of sepsis.
Nursing Home or Hospital Stays
Older adults who reside in nursing homes or who have been hospitalized are at a higher risk of developing healthcare-associated infections, which can lead to sepsis.
Invasive Procedures
Certain medical procedures, such as the insertion of catheters or intravenous lines, can increase the risk of infections and subsequent sepsis in the elderly.
By understanding these risk factors, caregivers can be proactive in monitoring the elderly for potential signs of sepsis and seeking prompt medical attention when necessary.
Early Detection and Warning Signs
Early recognition of sepsis is crucial in the elderly, as the condition can progress rapidly and lead to life-threatening complications. Caregivers should be vigilant for the following warning signs:
Sudden Changes in Mental Status
As mentioned previously, alterations in mental status, such as confusion, disorientation, or delirium, can be an early indicator of sepsis in older adults.
Fever or Hypothermia
Caregivers should closely monitor the patient’s temperature and be aware of both high and low readings, as they can both be signs of sepsis.
Rapid Breathing or Shortness of Breath
Difficulty breathing or increased respiratory rate can be a warning sign of sepsis-related respiratory distress.
Rapid Heart Rate or Low Blood Pressure
Caregivers should monitor the patient’s vital signs, including heart rate and blood pressure, as changes in these parameters can be indicative of sepsis-related cardiovascular instability.
Decreased Urine Output or Altered Kidney Function
Decreased urine output or changes in kidney function, such as increased levels of waste products in the blood, can be a sign of impaired kidney function due to sepsis.
Skin Changes
Caregivers should inspect the patient’s skin for signs of redness, warmth, rash, or mottled appearance, which can be indicators of sepsis-related skin changes.
Unexplained Fatigue or Weakness
Overwhelming fatigue or decreased physical activity in the elderly may be a warning sign of sepsis.
By being vigilant for these early warning signs and acting quickly to seek medical attention, caregivers can increase the chances of early detection and improve the patient’s chances of survival.
Treatment Options and Care Strategies
Prompt and appropriate treatment is essential for managing sepsis in the elderly. The treatment approach typically involves a combination of the following strategies:
Antibiotic Therapy
The cornerstone of sepsis treatment is the administration of broad-spectrum antibiotics to address the underlying infection. Caregivers should be aware that the elderly may require different antibiotic regimens or dosages due to age-related changes in drug metabolism and pharmacokinetics.
Fluid Resuscitation
Sepsis can lead to fluid and electrolyte imbalances, which may require intravenous fluid administration to restore and maintain adequate tissue perfusion and organ function.
Vasopressor Support
In cases of severe sepsis or septic shock, the use of vasopressor medications may be necessary to maintain blood pressure and ensure adequate organ perfusion.
Respiratory Support
Sepsis-related respiratory distress may require supplemental oxygen, mechanical ventilation, or other respiratory support measures to ensure adequate oxygenation.
Hemodynamic Monitoring
Close monitoring of the patient’s vital signs, including blood pressure, heart rate, and urine output, is essential to guide treatment and detect any deterioration in the patient’s condition.
Supportive Care
Comprehensive supportive care, such as management of underlying conditions, pain control, and prevention of complications (e.g., pressure ulcers, deep vein thrombosis), is crucial in the treatment of sepsis in the elderly.
Nutritional Support
Adequate nutrition is essential for the elderly with sepsis, as they may have increased nutritional requirements due to the metabolic demands of the infection. Caregivers should work closely with healthcare providers to ensure appropriate nutritional interventions, such as enteral or parenteral feeding.
Sepsis Bundles
Many healthcare facilities utilize evidence-based sepsis care bundles, which provide a standardized approach to the early recognition and management of sepsis. Caregivers should be familiar with their healthcare provider’s sepsis protocols to ensure timely and appropriate care.
Palliative and End-of-Life Care
In some cases, the elderly may not respond to treatment or may have underlying conditions that limit their ability to recover from sepsis. In these situations, palliative and end-of-life care may be appropriate to provide comfort and support to the patient and their family.
Caregivers play a crucial role in advocating for their elderly loved ones, ensuring that they receive prompt and appropriate treatment for sepsis. By collaborating closely with healthcare providers and being vigilant for early warning signs, caregivers can help improve the chances of survival and minimize the risk of long-term complications.
Preventive Measures and Best Practices
While sepsis cannot always be prevented, there are several measures that caregivers can take to reduce the risk of infection and subsequent sepsis in the elderly:
Vaccination
Ensuring that the elderly are up-to-date with recommended vaccinations, such as those for influenza and pneumococcal disease, can help prevent infections that can lead to sepsis.
Infection Prevention
Proper hand hygiene, wound care, and infection control measures, such as the use of personal protective equipment, can help prevent the development of infections that can lead to sepsis.
Prompt Treatment of Infections
Caregivers should be vigilant in monitoring the elderly for signs of infection and seek prompt medical attention to ensure appropriate treatment, reducing the risk of the infection progressing to sepsis.
Nutritional Support
Maintaining good nutritional status and hydration can help strengthen the elderly’s immune system and reduce their vulnerability to infections.
Mobility and Physical Activity
Encouraging regular physical activity and maintaining mobility can help prevent the development of infections, such as pneumonia or urinary tract infections, that can lead to sepsis.
Medication Management
Caregivers should work closely with healthcare providers to ensure appropriate medication management, including monitoring for any adverse effects or interactions that could increase the risk of infection or sepsis.
Chronic Disease Management
Careful management of underlying chronic conditions, such as diabetes, heart disease, or cancer, can help reduce the risk of infections and subsequent sepsis in the elderly.
Caregiver Education and Awareness
Educating caregivers on the signs and symptoms of sepsis, as well as the importance of early recognition and prompt treatment, can play a crucial role in improving outcomes for the elderly.
By implementing these preventive measures and best practices, caregivers can help protect the elderly from the devastating effects of sepsis and improve their overall health and well-being.
Conclusion
Sepsis is a life-threatening condition that disproportionately affects the elderly population, making it a critical concern for caregivers. By understanding the unique symptoms of sepsis in older adults, recognizing the early warning signs, and implementing appropriate preventive measures, caregivers can play a vital role in improving the chances of survival and reducing the risk of long-term complications.
Collaboration with healthcare providers, adherence to evidence-based protocols, and ongoing caregiver education are essential in the fight against sepsis in the elderly. By remaining vigilant and taking proactive steps to protect their loved ones, caregivers can help ensure that the elderly receive the timely and comprehensive care they need to overcome this serious medical condition.