As we age, our bodies undergo various changes, and one of the most concerning issues for the elderly is the increased risk of hip fractures. These debilitating injuries can have a significant impact on an individual’s quality of life, leading to reduced mobility, loss of independence, and even increased mortality rates. In this comprehensive guide, we will explore the causes and risk factors of hip fractures, the symptoms to watch for, immediate steps to take, treatment options, preventative measures, the role of nutrition and exercise, and long-term care and support for recovery.
Understanding Hip Fractures: Causes and Risk Factors
Aging and Bone Density Decline
As we grow older, our bones naturally lose density and strength, a process known as osteoporosis. This condition makes the bones more susceptible to fractures, especially in the hip region, which bears a significant amount of weight and stress during daily activities.
Muscle Weakness and Imbalance
Aging can also lead to a decline in muscle strength and balance, which can contribute to an increased risk of falls and, consequently, hip fractures. This is particularly true for older adults who are sedentary or have limited physical activity.
Chronic Health Conditions
Certain chronic health conditions, such as rheumatoid arthritis, Parkinson’s disease, and stroke, can increase the risk of hip fractures. These conditions may impair mobility, balance, and overall physical function, making the individual more prone to falls.
Medications
Some medications, such as corticosteroids, antidepressants, and certain seizure medications, can have side effects that increase the risk of falls and hip fractures. It is important for healthcare providers to carefully consider the potential risks and benefits of these medications in older adults.
Environmental Factors
The environment in which older adults live can also play a role in the risk of hip fractures. Factors such as poor lighting, uneven or slippery surfaces, lack of handrails, and the absence of assistive devices like canes or walkers can contribute to an increased risk of falls and subsequent hip fractures.
Nutritional Deficiencies
Inadequate intake of nutrients essential for bone health, such as calcium, vitamin D, and protein, can increase the risk of osteoporosis and hip fractures in the elderly.
Gender and Ethnicity
Women are at a higher risk of developing osteoporosis and, consequently, hip fractures, due to the hormonal changes associated with menopause. Additionally, certain ethnic groups, such as Caucasians and Asians, are at a higher risk of developing osteoporosis.
Recognizing the Symptoms of Hip Fractures

Sudden and Severe Pain
One of the primary symptoms of a hip fracture is sudden and severe pain in the hip or groin area. This pain may be accompanied by swelling, bruising, and limited range of motion in the affected leg.
Inability to Bear Weight
Individuals with a hip fracture often experience an inability to bear weight on the affected leg, making it difficult or impossible to walk or stand.
Shortened or Rotated Leg
In some cases, the affected leg may appear shorter or rotated in an unusual position compared to the uninjured leg, indicating a displaced fracture.
Difficulty Moving the Leg
Attempting to move the leg can be extremely painful and challenging for individuals with a hip fracture, as the joint may be unstable and the muscles surrounding the hip may be injured.
Shock and Confusion
The trauma of a hip fracture can sometimes lead to symptoms of shock, such as paleness, rapid breathing, and confusion, which require immediate medical attention.
Immediate Steps to Take After a Hip Fracture
Call Emergency Services
If you suspect that an individual has suffered a hip fracture, it is crucial to call emergency services or emergency medical personnel immediately. Prompt medical attention is essential for proper diagnosis and treatment.
Avoid Unnecessary Movement
Until medical help arrives, it is important to avoid unnecessary movement of the affected leg or hip. Gently stabilize the leg and hip using pillows or a blanket to prevent further injury.
Provide Pain Relief
If the individual is experiencing severe pain, you can provide pain relief by administering over-the-counter pain medication, if appropriate, or by applying a cold compress to the affected area.
Monitor for Complications
While waiting for medical assistance, monitor the individual for any signs of complications, such as shock, bleeding, or further injuries, and be prepared to provide emergency first aid if necessary.
Gather Relevant Information
If possible, gather any relevant information about the individual’s medical history, medications, and the circumstances of the injury, as this can assist the healthcare team in providing the best possible care.
Treatment Options: From Surgery to Rehabilitation
Non-surgical Treatment
In some cases, non-surgical treatment may be an appropriate option for hip fractures, particularly for stable, non-displaced fractures or for individuals who are not suitable candidates for surgery due to underlying health conditions.
Traction and Immobilization
Traction and immobilization techniques, such as the use of a splint or sling, may be employed to stabilize the fracture and alleviate pain while the bone heals.
Weight-bearing Restrictions
Patients may be required to limit or avoid weight-bearing on the affected leg during the initial stages of recovery, with the goal of gradually increasing mobility as the fracture heals.
Surgical Treatment
For many hip fractures, surgical intervention is the recommended course of action. The specific surgical procedure will depend on the type and severity of the fracture, as well as the individual’s overall health and medical history.
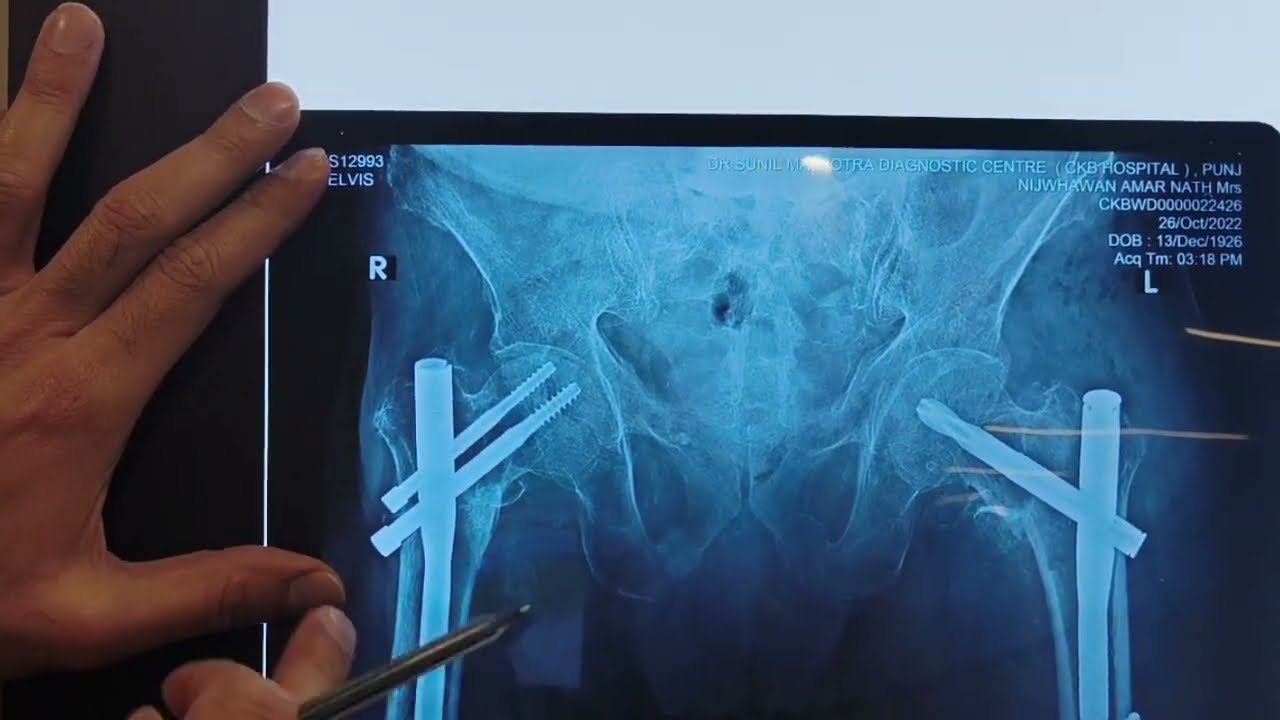
Internal Fixation
Internal fixation involves the use of metal screws, plates, or nails to stabilize the broken bone and facilitate healing. This approach is often used for stable, non-displaced fractures.
Arthroplasty
In cases of displaced or unstable fractures, or when the bone is severely damaged, a hip replacement (arthroplasty) may be performed. This involves replacing the damaged hip joint with an artificial prosthetic implant.
Minimally Invasive Techniques
Advances in surgical techniques have led to the development of minimally invasive procedures, which aim to reduce the impact on the surrounding tissues and promote faster recovery.
Rehabilitation and Recovery
Regardless of the treatment approach, a comprehensive rehabilitation program is essential for optimizing recovery and restoring function after a hip fracture.
Physical Therapy
Physical therapy plays a crucial role in the rehabilitation process, helping patients regain strength, flexibility, and mobility through a tailored exercise program.
Occupational Therapy
Occupational therapy focuses on helping patients adapt to daily activities and restore independence in their home environment, including the use of assistive devices and modifications to the living space.
Nutrition and Supplementation
Adequate nutrition, including sufficient protein, calcium, and vitamin D intake, is essential for bone healing and overall recovery.
Pain Management
Effective pain management, through a combination of medication, physical therapy, and other techniques, is crucial for enabling patients to participate actively in their rehabilitation.
Preventative Measures to Reduce the Risk of Hip Fractures
Bone Health Screening
Regular bone density scans, also known as dual-energy X-ray absorptiometry (DEXA) scans, can help identify individuals with low bone density or osteoporosis, allowing for early intervention and preventative measures.
Fall Prevention Strategies
Implementing fall prevention strategies, such as home modifications, the use of assistive devices, and regular exercise programs, can significantly reduce the risk of hip fractures in the elderly.
Home Safety Assessments
A professional home safety assessment can identify potential hazards and recommend appropriate modifications to the living environment, such as installing grab bars, improving lighting, and removing tripping hazards.
Balance and Strength Training
Engaging in exercises that improve balance, coordination, and muscle strength can help reduce the risk of falls and subsequent hip fractures.
Medication Review
Regularly reviewing and adjusting medications, in collaboration with healthcare providers, can help minimize the side effects that may increase the risk of falls and fractures.
Nutrition and Supplementation
Ensuring adequate intake of nutrients essential for bone health, such as calcium, vitamin D, and protein, can help maintain bone density and strength.
Calcium and Vitamin D Supplementation
For individuals who are unable to meet their calcium and vitamin D needs through diet alone, supplementation may be recommended.
Protein Intake
Adequate protein intake is crucial for the maintenance and repair of bone tissue, and older adults may require higher protein intakes to support bone health.
The Role of Nutrition and Exercise in Bone Health
Calcium and Bone Health
Calcium is the primary mineral component of bone and plays a crucial role in maintaining bone density and strength. Older adults should aim to consume the recommended daily intake of calcium, which is typically around 1,200 milligrams per day.
Vitamin D and Bone Health
Vitamin D is essential for the absorption and utilization of calcium, and it also plays a direct role in maintaining bone health. Older adults may require higher doses of vitamin D supplementation to maintain optimal levels.
Protein and Bone Health
Adequate protein intake is essential for the maintenance and repair of bone tissue. Older adults may require higher protein intakes, around 1.0 to 1.2 grams of protein per kilogram of body weight per day, to support bone health.
Weight-bearing Exercise and Bone Health
Weight-bearing exercises, such as walking, jogging, or strength training, can help stimulate bone formation and maintain bone density. Regular physical activity is essential for older adults to maintain strong, healthy bones.
Balance and Coordination Exercise
Exercises that improve balance, coordination, and muscle strength can help reduce the risk of falls and subsequent hip fractures in older adults.
Flexibility and Mobility
Maintaining flexibility and range of motion in the hip, leg, and core muscles can also contribute to better balance and stability, reducing the risk of falls and hip fractures.
Long-term Care and Support for Recovery
Rehabilitative Services
Ongoing rehabilitative services, such as physical and occupational therapy, are essential for helping older adults regain their mobility, independence, and quality of life after a hip fracture.
Home Modifications and Assistive Devices
Adaptations to the home environment, such as the installation of grab bars, ramps, and other assistive devices, can help facilitate independence and reduce the risk of future falls.
Community Support and Resources
Connecting with community-based support services, such as home health aides, meal delivery programs, and social activities, can provide valuable assistance and help older adults maintain their independence and social connections during the recovery process.
Caregiver Support
Providing support and resources for caregivers, such as respite care, support groups, and education on caregiving techniques, can help alleviate the burden and stress associated with caring for a loved one recovering from a hip fracture.
Long-term Follow-up and Monitoring
Ongoing follow-up with healthcare providers, including regular bone density scans, medication reviews, and assessment of overall health and function, is essential for monitoring and managing the long-term effects of a hip fracture.
Conclusion
Hip fractures in the elderly can be a significant and debilitating event, but with the right preventative measures, immediate care, and comprehensive rehabilitation and support, it is possible to maintain and improve quality of life. By understanding the causes and risk factors, recognizing the symptoms, and implementing effective treatment and preventative strategies, healthcare providers and caregivers can work together to protect the bone health and wellbeing of older adults. Through a combination of medical interventions, lifestyle modifications, and community-based support, individuals can overcome the challenges of a hip fracture and regain their independence and mobility.